From 24 March 2025 patients aged 18 and over attending the Emergency Department at Queen Alexandra Hospital will be offered opt-out testing for three types of viral infection:
- HIV
- Hepatitis B
- Hepatitis C
These are all infections which can be silent for many years. They can cause serious health problems if not treated, but very good medical treatments are available.
This testing is part of an NHS England programme that is already in place in many other Emergency Departments including those in London, Brighton and Manchester. It is part of a national project to stop any new infections with these viruses by 2030.
What does this mean for you?
Anyone aged 18 or over who has a blood test in the Emergency Department will also have their blood tested for HIV, Hepatitis B and Hepatitis C.
We will only contact people with positive results. If this is the case for you, one of our medical teams will be in touch to discuss your results and what happens next.
If your tests are negative, the results will be in your medical notes and accessible by your GP. We will not contact you about them. In this case, no news is good news. If you would like to check your results, please contact your GP at least 14 days after your test.
Where can you find out more information?
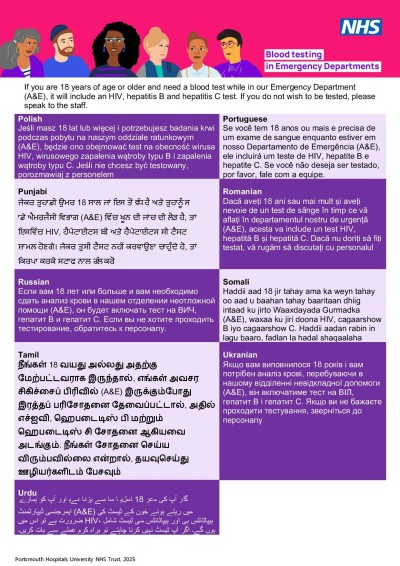
Written information on this testing is also on posters and leaflets in the Emergency Department. Leaflets in the most spoken languages in our communities are available.
If you do not wish to be tested, please tell the staff member taking your blood. If you choose not to be tested, this will not change how we look after you.
If you have any concerns or questions, you can contact our Microbiology Team via email: pho-tr.
Many people can have these viruses without any symptoms. They can remain silent for a long time and cause damage. Without treatment they can lead to serious long-term problems, like liver damage and cancer. Finding and treating viruses early helps to control or cure them and stops them causing more damage. People on treatment are also less likely to pass their infection onto others.
Let the person taking your blood know that you do not wish to be tested, there is no pressure to have this done and it is your choice.
This is part of a national programme to stop the spread of HIV, Hepatitis B and Hepatitis C by finding people living with these infections and engaging them in care. The UK is committed to ending new infections with these viruses by 2030.
Testing in Emergency Departments is one of many approaches which supports the HIV Action Plan (aligned to the World Health Organisation (WHO) and UNAIDS global HIV strategies), and the WHO viral hepatitis elimination goals. It is an inclusive and population-focused approach to prevention, which benefits individuals, the public and the NHS.
If your test result positive or you need a retest, then you will be contacted by a member of the clinical team who will arrange for you to have further blood tests to either confirm or rule out that you have a blood borne virus. If your result is positive, either from the initial tests or after further tests, they will arrange for you to see the correct specialists and make sure that you understand everything.
We will try at least three ways to contact you. In the following order:
- Telephone call: please be aware when you get a phone call from the hospital, it usually appears as a withheld (private) number, and we cannot leave confidential information on voicemail messages. Please consider answering calls from withheld numbers for the 14 days after you attended the ED.
- Confidential letter to your home address.
- Through your GP – a confidential letter will be sent to your GP.
If your test is negative, we won’t contact you. If you would like to check your results, please contact your GP (at least 14 days after your test). If you do not have a GP, you can find one here.
The Hepatology team (for Hepatitis), or Sexual Health Services (for HIV) will be able to provide you with different options for support during your healthcare journey. Care and treatment is safe, effective and free from the NHS.
Community support is available, these are volunteers who have lived with and overcome these illnesses. They are on hand to offer support, guidance and practical advice if you need it via SMS, email, telephone or face to face.
All adults who attend the Emergency Department and have a blood test will be routinely tested for blood borne viruses unless they opt-out. If you have been offered a test before this will be recorded on your medical record. If you have another blood test in the emergency department the 12 months after this, the IT system will alert your healthcare professional that you have previously been offered a test and they can manually opt you out of blood borne virus testing.
We are working on a digital solution to make this automatic, so that you are only offered these tests every 12 months. For now, we ask that you let your health care professional know if you do not wish to be tested for blood borne viruses every time you have a blood test in the Emergency Department.
Yes. If you have previously opted out but now wish to be tested, please let a member of staff know so that if we are testing your blood on a different visit, we can arrange these tests for you.
It is important to know that tests taken as part of the screening programme will be available for your GP as part of your health record. If you would prefer your GP not to know these results, then you may wish to “opt out” of having these tests in the Emergency Department.
If your test is not negative, our clinical teams will reach out to you first. After this they will arrange any necessary repeat tests and coordinate a referral with the appropriate service. This will mean sharing your details with the appropriate services. Your data will be kept confidential and only shared with other healthcare professionals when necessary for your care.
It is important that you are aware of your own results so that you can access appropriate care. Therefore, if it has not been possible to contact you directly, we will contact other suitable healthcare professionals (such as your GP, the homeless healthcare team or drug and alcohol services) to link you into the specialist services and provide any peer support needed. Hepatitis B and C are both notifiable diseases in the UK which means we will also need to inform the UKHSA health protection team who work with local teams to prevent future infections.
If you don’t have an emergency, please do not attend the emergency department. If you wish to be tested for one of these viruses, then contact your GP or local sexual health service who can arrange this for you. Online and in person tests are available for people who live in Hampshire, Southampton, Portsmouth and Isle of Wight, find more information, make an appointment or order an online test today. If you don’t live in the area, you can still access online free home testing kits for Hepatitis C and for HIV.
Yes, without treatment there is a chance that these viruses can be passed onto others by bodily fluids. With treatment, the chance of passing them onto others significantly reduces.
Online and in person tests are available for people who live in Hampshire, Southampton, Portsmouth and Isle of Wight via local sexual health services, find more information, make an appointment or order an online test today. If you don’t live in the area, you can still access free home testing kits for Hepatitis C and for HIV. Alternatively, you can get in person testing at your GP surgery or local sexual health service.
We would still recommend you get tested today, but we would suggest you also contact our local sexual health service who can provide you advice and arrange further tests in a few weeks’ time.
HIV (human immunodeficiency virus) is a virus that attacks the body’s immune system (our natural defence against infection and disease). In late-stage HIV infection, also known as AIDS, the weakened immune system means the body is more vulnerable to life-threatening conditions such as pneumonia and cancer.
HIV can affect anyone, regardless of gender or sexual preference. In 2019, around 38% of people newly diagnosed got HIV through heterosexual sex and 41% through sex between men.
Nearly 1 in 16 people who have HIV in the UK don't know that they have the virus. But for the 94% that do, life-saving HIV treatment and care can be accessed at any UK HIV clinic. Anti-HIV drugs are sometimes called combination therapy because people usually take three different drugs at the same time – often combined into one table.
Taking HIV treatment every day can supress the virus to a level where it cannot be detected and cannot be passed on. This is why getting tested for HIV is so important – you can start treatment straight away, protect your health and not pass the virus on.
More information on HIV is available here. More information on the local services for HIV is available here.
Hepatitis B, sometimes called ‘Hep B’ or ‘HBV’, is a virus that infects the liver. Hepatitis B is the most widespread form of hepatitis worldwide. Most people clear the virus by themselves, and it has no lasting effects. But in some people hepatitis B infection becomes long term (chronic). If this happens, it can lead to liver damage, liver cancer or liver failure.
Most people living with hepatitis B got the virus when they were born or as a young child. There is more chance of this happening in countries with higher levels of hepatitis B (the UK is not one of them). The virus is spread through blood and other bodily fluids. This means it can be passed from a mother to her baby. It can also be passed on during sex, or by sharing any items that can get blood on them, such as razors or needles for injecting medicine or drugs.
There is no cure for hepatitis B yet, but there are treatments available that can manage the condition. Drug treatment for hepatitis B is taken in tablet form once a day. Treatment makes you less likely to get serious liver disease and can also reduce the levels of the virus so that you cannot pass it on. There is also a vaccine for hepatitis B that can stop your close contacts, such as others in your household, from getting infected.
More information on HBV can be found here.
Hepatitis C (HCV) is a virus that infects the liver. Without treatment, hepatitis C can cause serious damage to the liver and may eventually lead to cirrhosis, liver cancer or liver failure. With treatment, it’s usually possible to cure hepatitis C after just a few months.
There are two stages of hepatitis C:
-
- Acute hepatitis C – diagnosed within the first six months of the infection
- Chronic hepatitis C – diagnosed after the first six months of the infection
If you have been diagnosed with acute hepatitis C, your healthcare professional may recommend treatment or wait to see whether your body is able to clear the infection naturally. Around one in five people with acute hepatitis C can clear the infection this way. If your healthcare professional has suggested this approach, you should have a blood test a few months after you have been diagnosed to see whether your body has cleared the virus on its own. However, if this has not worked, you should start a course of treatment. If you have been diagnosed with chronic hepatitis C, treatment should begin as soon as possible.
Hepatitis C is curable. Almost all (97%) people who receive treatment for hepatitis C make a full recovery. Drug treatment for hepatitis C is taken in tablet form, typically for between 8 to 12 weeks. There are several different drug treatments for hepatitis C. Older treatments used something called interferon, which could make you feel like you had the flu, the current treatments are interferon-free. The treatment your specialist care team recommend will depend upon how long you have had the virus, your health, your wishes and the genotype (variation) of the virus.
More information on hepatitis C can be found here.